Are you having problems coming off the pill?
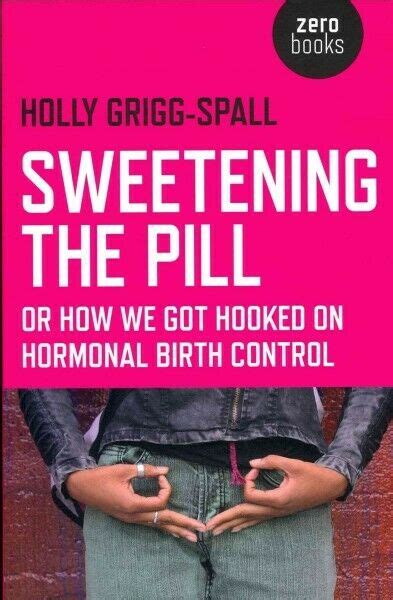
The medical approach to period problems shuts ovulation with contraceptives such as the Pill, implants, injections and Nuvaring.
As ovulation stops, so the production of DHEA, oestrogen, progesterone shuts down as well. It causes the ovaries to shrink by almost 50%, to the same size that they shrink to at menopause. When HBC is discontinued, the ovaries previously suppressed with synthetic hormones fail to return to healthy function, often leading to irregular periods, heavy bleeding and acne.
In the meantime the hormonal imbalances cause troubling and potentially serious side effects such as depression, weight gain, microbiome disturbance, and loss of libido.
Emerging research is also suggesting long term impacts on insulin resistance, fat mass, diabetes and bone mass.
What is hormonal birth control?
Our natural hormones oestrogen, progesterone an DHEA are required to make a healthy brain, bones, muscles and metabolism.
- Estradiol (the main oestrogen) plays a key role in insulin signalling;
- Estradiol and progesterone influence the release of neurotransmitters – serotonin, dopamine, GABA – to keep your mood stable throughout the cycle;
- Progesterone converts to alloprogesterone and interacts with the brain and nervous system to relax and keep your mood stable coming up to your period.
The steroids in HBC are not the same as our natural hormones.
- Natural oestrogen is replaced by Ethinyl estradiol which worsens insulin sensitivity, causing insulin resistance and weight gain.
- Natural progesterone is replaced with a variety of progestins
- Levonorgestrel causes abortions – it is used in the Plan B abortion pill
- Many synthetic progestins have a similar structure to testosterone, and are androgens i.e. they work as testosterone
- Natural progesterone is a calming hormone which converts to allopregnenalone, which is a strong modulator of the GABA receptors in the brain. It is hormonal valium. Progestins don’t convert to allopregnenalone and so don’t support mood or brain function. Levonorgestrel dramatically reduces progesterone and therefore allopregnenalone, and does the opposite, reducing GABA receptors, leading to anxiety.
Synthetic Progestins increase testosterone
Progestins have an androgen index, indicating how close their effects are to testosterone. Androgenicity is described as the progestin’s affinity for and binding to the androgen receptor, and it’s effect on the sex hormone binding globulin (SHBG). SHBG binds testosterone and estrogen making the sex hormones unavailable for use at the receptors.
Levonorgestrel and dl-norgestrel have a high affinity for sex hormone binding globulin and decrease free sex hormone binding globulin levels by binding it and displacing testosterone, consequently increasing free testosterone levels. (PMID: 15802398)
High androgen index:
- Causes acne, weight gain, anxiety and hair loss (can be devastating)
- Older progestins are made from testosterone
- Progestins include: Levonorgestrel, Norgestrel, Medroxyprogesterone
- Included in: Levelen, emergency contraception, Mirena, Depo-provera
Medium androgen index:
- Norethindrone, Desogesterel, Etonogestrel
- Included in: Loestrin, Implanon, Nova ring
Low androgen index:
- suppress DHEA, higher risk of fatal blood clots, depression and anxiety, loss of libido
- Drospirenone – derived from a diuretic drug – anti-androgen – reduces acne but causes more depression, anxiety and clot risk than the high androgen progestins
- Cyprotenone – Yaz and Yasmin, Brenda
Mirena coil
- It is an intrauterine Levonorgestrel releasing IUD
- Works locally in the uterus, prevents fertile mucus, impairs sperm and thins the uterine lining.
- Blood levels of progestins are at 10% compared to Levonorgestrel pill, but this is still enough to cause androgen side-effects in some women such as acne and hair loss.
- Allows normal estradiol and some ovulation .
Side effects of taking HBC
- Altered microbiome of gut
- Altered microbiome of vagina
- Altered brain structure
- Altered sleep architecture
- Reduced bone density
- Gallbladder disease
- Increased risk of cervical dysplasia
- Increased risk of autoimmune disease
- Zinc deficiency
- 3-fold higher risk of breast cancer
- Digestive bloating
- Recurrent bladder infections
- Thrush
- Vaginal dryness
Side effects of stopping HBC
A real period is about the healthy functioning of the ovaries and the healthy production of oestradiol and progesterone via ovulation. A pill bleed suppresses those hormones and instead is a bleed from the withdrawal of the drugs. So the timing of the pill bleed is about the dosing of the drug.
There is no medical reason to bleed monthly on HBC. Hence HBC does not regulate periods. It stops periods altogether, and a bleed only occurs when HBC is paused which causes a drug deficiency.
Once HBC is stopped, the most common symptoms are:
- Irregular or skipped periods
- Heavy menstrual bleeding
- Ovulation pain and menstrual cramps
- Acne breakouts
- Bloating
- Mood swings
My approach to coming off HBC easily
I support women in coming off hormonal birth control to minimise unwanted side effects such as rebound acne, irregular periods or no periods. Additionally she provides support for weight loss and hair growth.
My approach is tailored to each woman. Hormonal birth control does not fix period problems, only masks them so support is customised depending on the health issues before starting hormonal birth control.
My approach to coming off the pill consists of consecutive stages, and ideally should begin 2-3 months before HBC is stopped:
- Address health issues masked by HBC:
Individualised support, with 4 distinct strategies, depending on how periods were before HBC started:
- PLAN A: normal periods
- PLAN B: irregular periods
- PLAN C: acne
- PLAN D: heavy bleeding and/or period pain
- Support nutrition:
- Individualised recommendations for appropriate nutrition, including avoiding sugar and dairy increasing healthy fats, protein, fibre and phytonutrients.
- Full blood tests including: liver function, thyroid metabolism, iron levels, vitamin D, vitamin B12, folate, cholesterol, zinc levels.
- Recommend appropriate supplements
Individualise supplementation of all the nutrients that HBC depletes including:
- B vitamins: loss of B vitamins can lead to depression, which then leads women to be prescribed anti-depressant medication (if you would like support with coming off anti-depressants then please mention this at your discovery call).
- Magnesium
- Zinc
- Vitamin D, which declines once off HBC, and is required for ovulation
- Support the hypothalamic pituitary ovarian axis with glandulars to revive the ovaries, restore ovary-brain communication and support fertility.
- Test hormones periodically
- 3 months after coming off HBC, testing for oestradiol, progesterone and testosterone is recommended, to make any further adjustments to your protocol.
- Some women may need cortisol tests.
- Support you while your periods normalise and symptoms reverse
How long will it take for periods to resume and normalise?
How long it takes for periods to resume and normalise depends on which HBC was taken, how long it was taken for, what it was taken for originally and your age.
- Stopping the Pill should allow the ovaries to return to their normal size within 3 months, and AMH levels to normalise within a year. Which means that conception can be delayed for over a year.
- It can take up to 18 months for cycles to return after Depo-Provera discontinuation
- IUD can allow a quick return of fertility, but progestin-based IUDs can take longer.
The wonderful news is that I can guide and support you with nutrition, supplements and lifestyle changes to restore ovarian function and get you back to your natural flow.