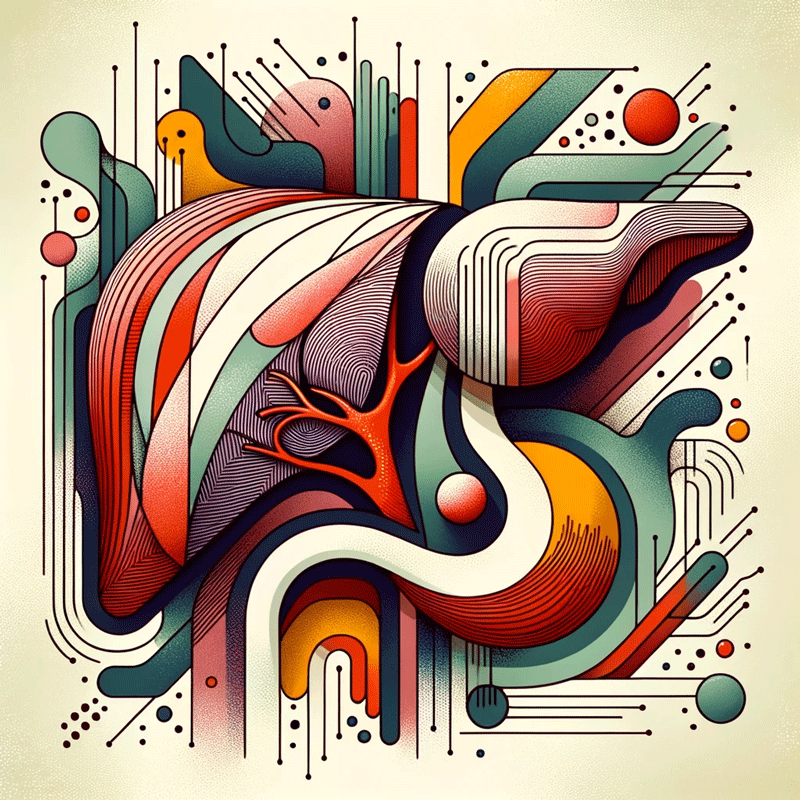
If you’ve ever felt a sharp, cramping pain under your ribs on the right side of your abdomen, it likely signals a problem with your gallbladder. The gallbladder is a small organ that stores and concentrates bile created by the liver. Bile helps digest fats from the foods we eat. Issues like gallstones or inflammation can prevent proper bile flow and cause gallbladder pain.
Gallstones form when hardened deposits of cholesterol and bile salts build up in the gallbladder or bile ducts. These stones irritate the gallbladder wall, which can trigger painful spasms. Gallstones also block the release of bile, causing it to back up into the gallbladder. This added pressure on the organ results in the agonizing pain under the ribs. This same pain can be referred to an area between the shoulder blades.
In addition to gallstones, inflammation from infections, bile duct issues, and other gallbladder diseases can all impair its ability to release bile. Without enough bile, the gallbladder never fully empties and bile becomes sludgy and concentrated. The excess bile can also crystallise into new gallstones, fuelling the problem.
Symptoms of an underperforming gallbladder extend beyond pain under the ribs. Some other signs include constipation, indigestion after meals, bloating, light coloured stools, nausea, and vomiting.
Making dietary changes to maintain bile flow may help relieve gall bladder pain. These include eating bitter herbs, staying hydrated, and limiting processed foods. Supplements that include whole beet concentrate like BetaTCP can improve the flow of bile in a few days, clearing the pain and improving digestion.
Don’t ignore recurring pain under your ribs as it often indicates problems in the biliary system.