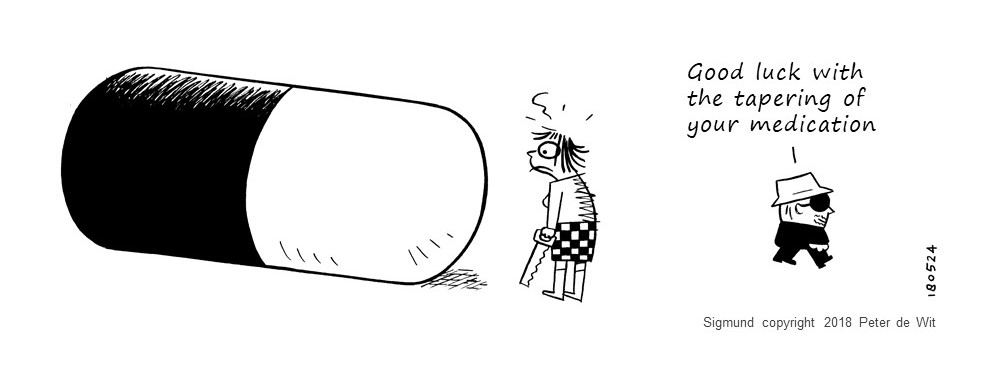
In a new article in European Neuropsychopharmacology, researchers Mark Horowitz and David Taylor provide guidance for tapering psychiatric drugs, whether for full discontinuation or to reduce the dose. They suggest a slow, individualized taper to minimize withdrawal effects.
“The general principle when reducing or stopping psychiatric medications is as follows. Make a small reduction, monitor for withdrawal effects or destabilization of the patient, then ensure stability before making further reductions. Reductions should probably be made in smaller and smaller increments because of the pharmacology of the drugs; the final dose before completely stopping will need to be very small.”
Horowitz and Taylor have previously written about this approach for antidepressants in Lancet Psychiatry and for antipsychotics in JAMA Psychiatry (with Sir Robin Murray).
…Some people may require months or even years to slowly decrease their dose before eventually stopping the drug. The researchers write:
“Withdrawal effects (and relapse) might be minimized by stopping psychiatric drugs over a period long enough for underlying adaptations to the drug to resolve.”
According to the researchers, based on studies of the drugs’ effects on the brain, psychiatric drugs impact the brain along with a hyperbolic relationship. That is, at low doses, small adjustments have huge impacts—but at high doses, even large adjustments have less of an impact.
“The relationship between dose of a psychiatric drug and its effects is hyperbolic,” they write. “This is a consequence of the law of mass action: when there are few molecules of a drug present at the site of action, every additional molecule has a large incremental effect, but when higher concentrations are present each additional molecule has less and less effect, as receptors become saturated.”
This means that dose reductions should not be linear (reduced by the same amount each time, e.g., 40, 30, 20, 10, 0 mg). Instead, one strategy is to reduce the current dose by 10% each time, especially ensuring that the last adjustment—to full discontinuation—is very small.