Are you experiencing changes in your body that you can’t quite explain? Feeling like you’re on an emotional rollercoaster? It might be perimenopause, the transitional phase leading up to menopause. Understanding the signs and symptoms can help you navigate this natural and inevitable part of your life.
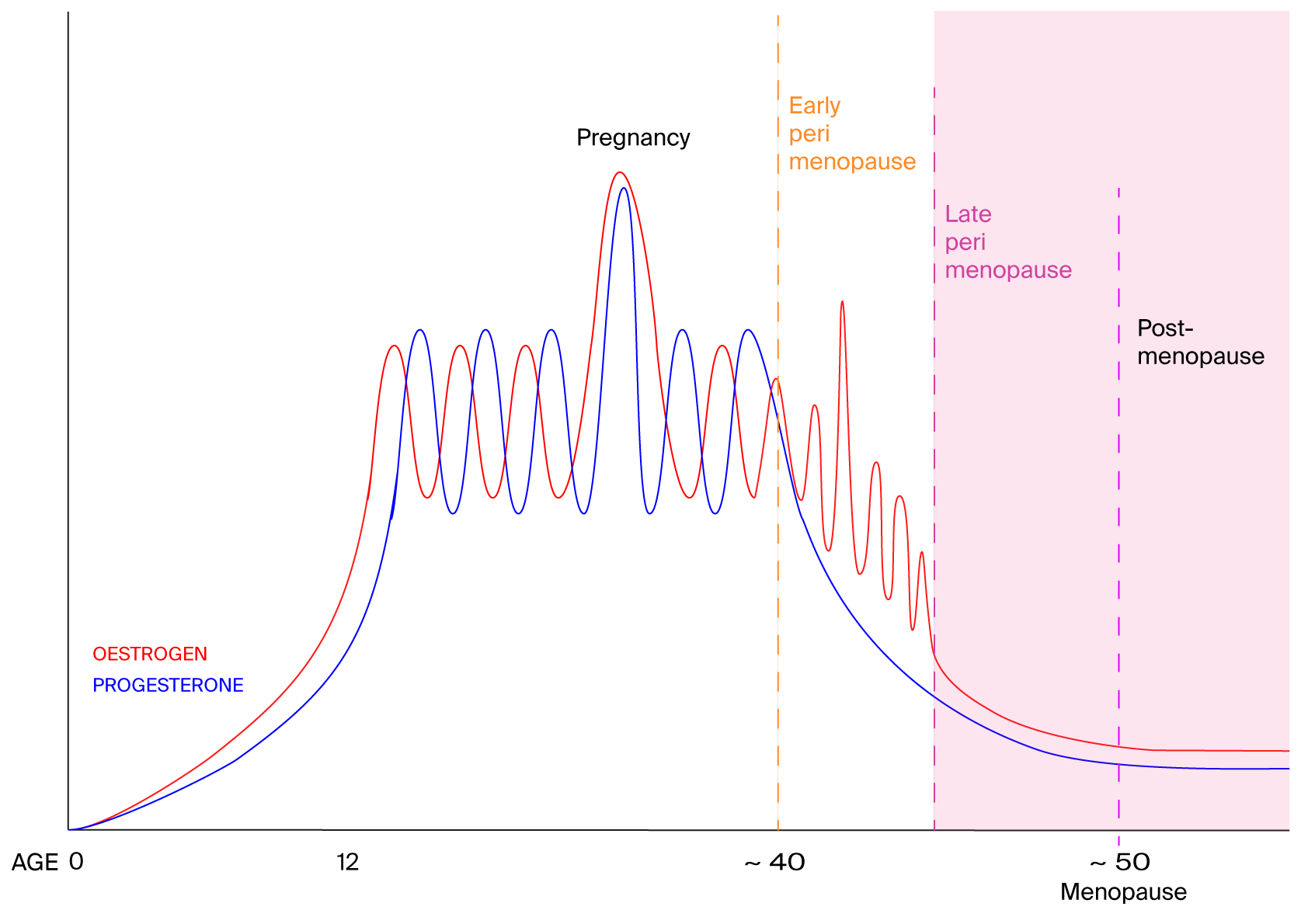
During perimenopause, which typically starts in our 40s but can happen as early as the 30s, the ovaries gradually produce less oestrogen. This hormonal shift can cause a range of physical and emotional changes. Common symptoms include irregular periods, hot flashes, night sweats, mood swings, fatigue, and a decreased sex drive. The average duration is three to five years, although it can last just a few months or extend as long as a decade.
Through my clinical work I have defined 4 stages in the menopausal transition, but first let’s go through a quick overview of the menstrual cycle.
The roles of oestrogen and progesterone in our menstrual cycle
During our peak reproductive years, the amount of oestrogen and progesterone in circulation rises and falls fairly predictably throughout the menstrual cycle. Oestrogen thickens the uterine lining – this becomes the blood flow of your period, and it stimulates ovulation. After ovulation (14 days before your period) the empty follicle from which the egg was released forms a structure called the corpus luteum. The corpus luteum produces progesterone during the luteal phase, the second half of your cycle. Progesterone keeps the lining stable and prepares it for implantation during the second half of your cycle. A drop in progesterone at the end of your cycle signals to your body that it’s time for your period to begin.
4 stages in the menopausal transition
The transition to menopause via perimenopause is a natural phase in our lives, characterised by hormonal fluctuations which can lead to a variety of symptoms that may affect your physical and emotional well-being.
1. Early perimenopause: oestrogen dominance
As our egg supply is slowly decreasing, we start skipping ovulation. This means oestrogen is still produced which thickens the uterine lining, but because ovulation doesn’t happen, we don’t get the progesterone we need to balance oestrogen. This means that
- periods come closer together
- periods get heavier, some women experience flooding.
Unbalanced oestrogen can also lead to
- breast pain,
- fibroids,
- anxiety,
- bloating,
- headaches
- worsening of endometriosis and PCOS
In the meantime low progesterone can cause
- anxiety,
- low moods and mood swings.
- depressive feelings
- insomnia or other sleep problems, because progesterone acts as a sedative
2. Late perimenopause: oestrogen decline
As oestrogen is falling,
- periods are coming further apart
- bleeds are lighter
- common menopausal symptoms start: hot flushes, night sweats, weight gain, brain fog, memory problems, fatigue as well as joint pain, dry eyes (read more about it here and here).
3. Menopause
This last just 1 day, the anniversary of the last period you had 12 months ago.
4. Post-menopause
The time after menopause is post-menopause. Many women ask when menopause ends – officially menopause only lasts one day, but being post-menopausal doesn’t end as that is the stage we are in forever after menopause. What they are really asking is when will this nightmare end? The typical symptoms that started in late perimenopause are getting worse and can continue for another 10 – 15 years or longer. Vaginal dryness is common as are urinary tract infections (read more about it here and here).
How to tell if you’re perimenopausal
Ask yourself these questions,
Am I still having periods?
- yes and your last period was within the last 12 months, you are perimenopausal
- No and your last period was more than 12 months ago, you are post menopausal
If you’re still having periods, and they are:
- heavier? This means you are coming up to early perimenopause
- coming closer together and are heavier? This means you are in early perimenopause
- coming further apart and are lighter? This means you are in late perimenopause
Of course we all different, and we can respond differently to our hormonal fluctuations, but the answers to these questions can give you a general idea of where you are in the transition.
Functional medicine approaches to smooth the transition and beyond.
The transition to menopause can be a bumpy ride and it can get bumpier still post-menopause. My approach in early perimenopause is to support oestrogen detoxification as efficiently as possible, to reduce oestrogen dominance as much as possible. Many of us have problems with oestrogen detoxification because it is a metabolically complex system involving the liver, blood sugar, cortisol, optimal vitamins and minerals, and the gut microbiome to name just a few players. Do get in touch if you’d like to have a chat about a personalised health plan to support your early transition, especially because this process can last for 5 years or more.
For late perimenopause and post-menopause I have developed a nutritional solution that is tailored to each woman and reverses all the symptoms over 5 weeks. This approach is based on the fact that oestrogen and insulin work together to extract energy from sugar and carbohydrates, so when oestrogen declines insulin becomes dominant, and without it’s partner it converts sugar and carbs to fat, and stops fat burning. When you can’t burn sugar or fat, starvation sets into the body and the brain. This leads to hot flushes, night sweats, brain fog, anxiety, low moods, fatigue, weight gain. My Menopause Core Nutrition Solution addresses these metabolic imbalances directly with food alone and also allows for food personalisation so that you know what you should be eating now and in the future to prevent these symptoms from returning. The course is on special offer until November 10th, have a look and see if it’s right for you.