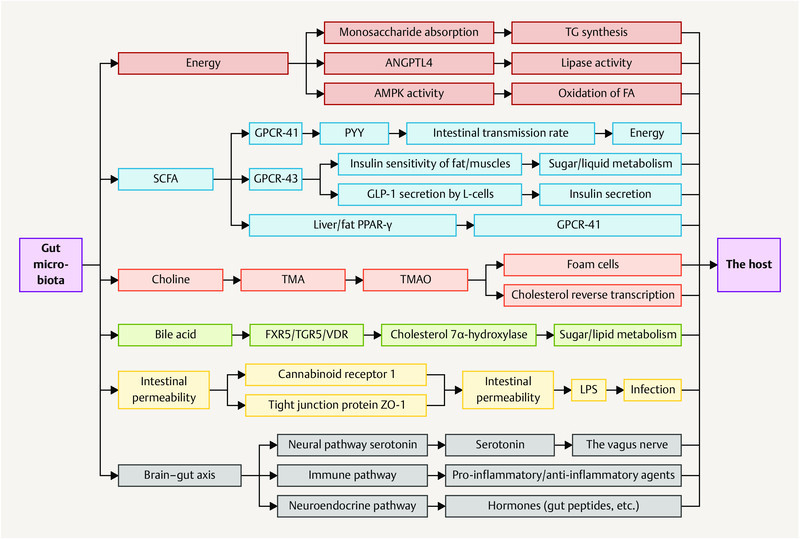
Nuclear receptors (NRs) are a superfamily of transcription factors induced by ligands and also function as integrators of hormonal and nutritional signals. Among NRs, the liver X receptors (LXRs) and farnesoid X receptor (FXR) have been of significance as targets for the treatment of metabolic syndrome-related diseases. In recent years, natural products targeting LXRs and FXR have received remarkable interests as a valuable source of novel ligands encompassing diverse chemical structures and bioactive properties. This review aims to survey natural products, originating from terrestrial plants and microorganisms, marine organisms, and marine-derived microorganisms, which could influence LXRs and FXR. In the recent two decades (2000–2020), 261 natural products were discovered from natural resources such as LXRs/FXR modulators, 109 agonists and 38 antagonists targeting LXRs, and 72 agonists and 55 antagonists targeting FXR. The docking evaluation of desired natural products targeted LXRs/FXR is finally discussed. This comprehensive overview will provide a reference for future study of novel LXRs and FXR agonists and antagonists to target human diseases, and attract an increasing number of professional scholars majoring in pharmacy and biology with more in-depth discussion.
Astragalus:
Astragalus membranaceus (Fisch.) Bunge, widespread in Europe and Asia, is beneficial to the treatment of diabetes, hyperlipidemia, atherosclerosis, and cancers, with its key constituents like astragaloside IV and cycloastragenol (164). Compound 164 stimulated FXR transcription activities and regulated the expression of FXR target gene in HepG2 cells as a potential candidate for NAFLD. Meanwhile, it improved metabolic profiles, ameliorated hepatic steatosis, altered BA composition, and activated FXR signaling and feedback loops in diet-induced obesity mice, further confirming the promise in ameliorating NAFLD. Besides, 164 also alleviated hepatic steatosis in methionine and choline-deficient L-amino acid diet-induced NASH mice (Gu et al., 2017b).
Guggulsterone:
Guggulsterone, existing in two isomeric forms, namely, E-guggulsterone (234) and Z-guggulsterone (235), is the active agent isolated from the resin of Commiphora mukul (Arn.) Bhandari, responsible for antihyperlipidemic effect. E/Z-guggulsterones 234 and 235 have been identified as FXR antagonists directly, to decrease hepatic cholesterol levels in rodent models. Moreover, Z-guggulsterone (235) exhibited remarkable FXR antagonism with an IC50 of 1–5 μM in HepG2 cells, increased the cholesterol CYP7A1, and further decreased the circulating cholesterol level (Urizar et al., 2002; Urizar and Moore, 2003; Bhutani et al., 2007; Yu et al., 2009; Singh and Sashidhara, 2017).
Hesperidin:
A flavanone glycoside abundantly found in lemons and oranges is hesperidin (183), treatment with which prevented cholestatic liver injury and reduced BA toxicity in HepaRG cells via activating FXR. Compound 183 dose-dependently protected against 75 mg/kg dose of ANIT-induced cholestasis and liver injury as reversing increases in the liver index, biliary index, serum AST, ALT, alkaline phosphatase, and total bilirubin, functioning as an effective agent for the prevention and therapy of cholestatic liver disease (Zhang et al., 2020a).
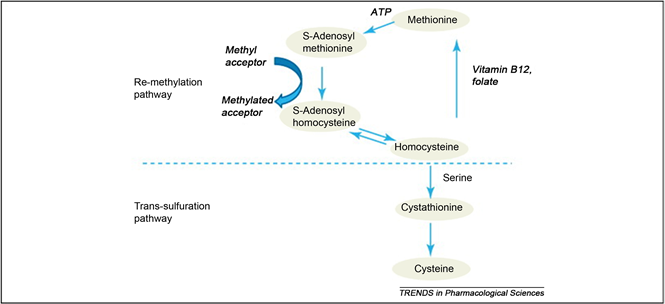
Betaine:
Betaine (104), a natural trimethyl glycine in common foods, including wheat products, spinach, pretzels, and shrimp, has been used for the therapy of NAFLD via upregulating hepatic expression of LXRα and PPARα, along with attenuating the changes in their associated target genes in fructose-induced rat models. 101 also ameliorated hepatic lipid accumulation, gluconeogenesis, and inflammation through a battery of determinations, further confirming potential mechanisms involved in the treatment of NAFLD (Ge et al., 2016; Chen Q. et al., 2017).
Allicin:
Allicin (105) is an essential ingredient of garlic, responsible for its favor, and its pharmacological activities range from anti-inflammatory to antioxidative stress and antihypertensive activities. 105 has also been confirmed to attenuate inflammation via increasing the expression of LXRα in a dose-dependent manner (Zhang et al., 2017).
Taurine:
Taurine (106), known as 2-aminoethanesulfonic acid is synthesized in the liver to a small extent, which is also isolated from seafood. Macrophage cells incubated with 106 inhibited cholesterol accumulation and regulated genes expression involved in RCT as an LXRα agonist (Hoang et al., 2012c).
Luteolin:
Luteolin (118), occurring in a broad range of vegetables, fruits, and grains like carrots, peppers, celery, parsley, and spinach, is a common dietary flavonoid exerting numerous biological activities including antioxidant, anticancer, antimicrobial, antiallergic, and antiinflammatory effects. It abrogated agonist-induced LXRα/β transcriptional activity and suppressed the expression of related target genes serving as an LXRα/β antagonist (Francisco et al., 2016). Treatment with 118 inhibited LXR activation in HepG2 cells and eliminated lipid accumulation induced by LXR-SREBP-1c activation, thereby decreasing TG accumulation and primary hepatocytes. Overall, lipid accumulation induced by LXRs-SREBP-1c activation was abolished both in vivo and in vitro after treatment with 118, indicating the potential as a therapeutic agent for treating NAFLD (Yin et al., 2017). Besides, 118 in combination with cisplatin could potentially be used as a new regimen for the treatment of ovarian cancer (Wang et al., 2018c). It exhibited that 118 could upregulate LXRα and downstream target gene expression to control cholesterol metabolism (Park et al., 2020).
Curcumin:
Curcumin (133), an active phenol derivative obtained from Curcuma longa L., could suppress the hepatic overexpression of LXRα, PPARγ, and fatty acid synthase. An immunoblot analysis also verified that 133 decreased the protein expression of LXRα and SREBP1c in the liver. Moreover, histological and serum biochemical analyses indicated that 133 apparently attenuated the hepatic lipid accumulation and decreased TG, TC, and nonesterified fatty acid levels in NAFLD mice model on account of the role for the prevention and treatment of NAFLD (Maithilikarpagaselvi et al., 2016; Chen et al., 2017b; Auger et al., 2018).