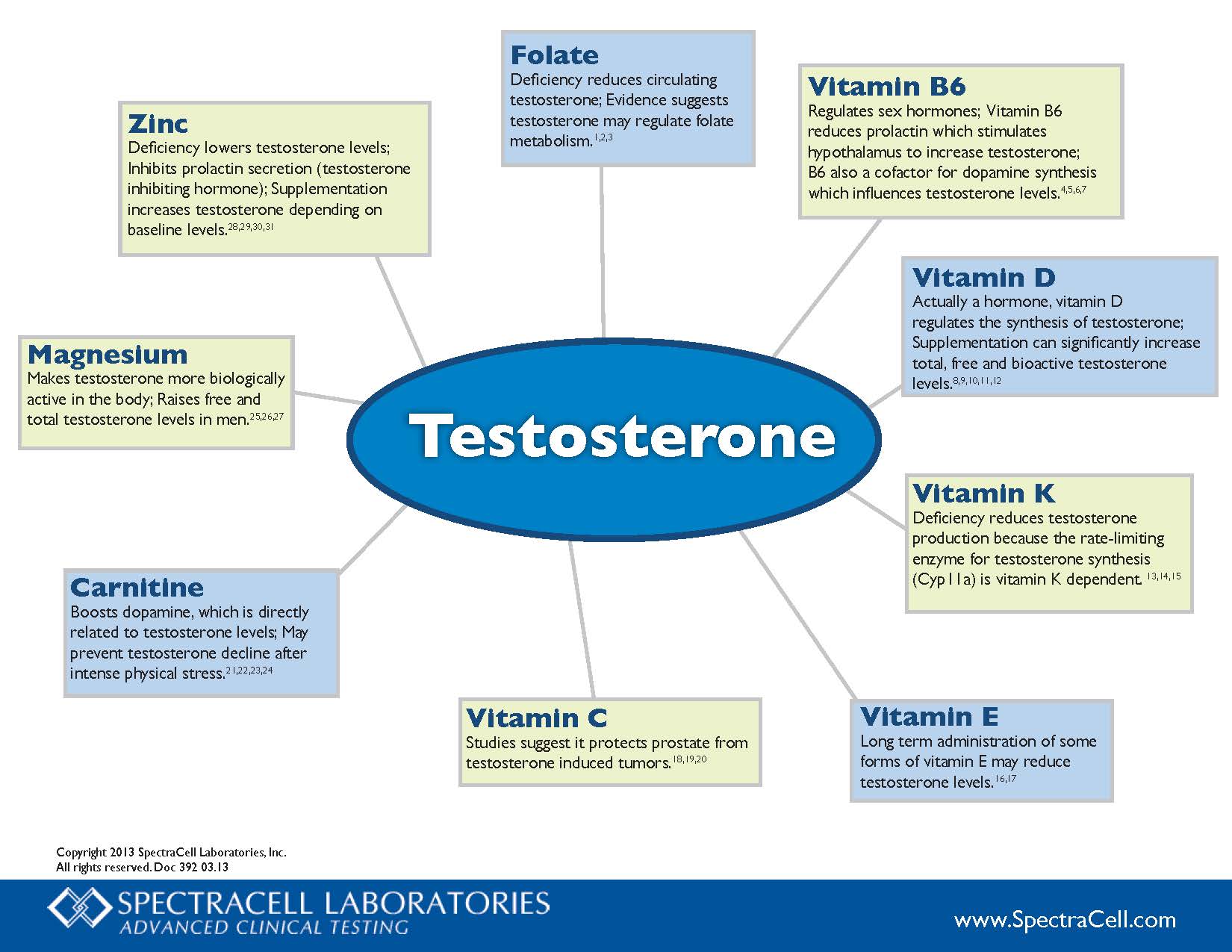
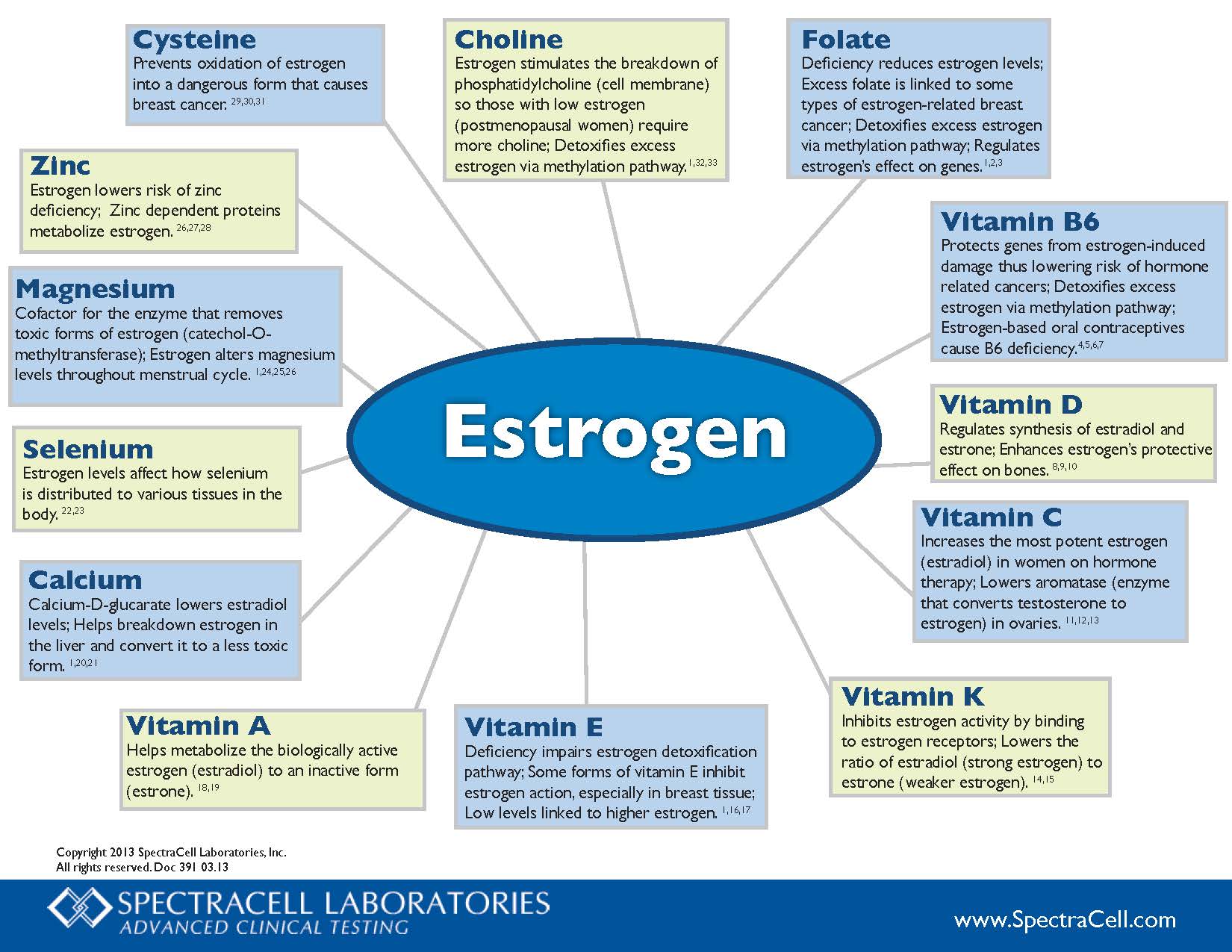
One of the more pervasive, and frankly, annoying myths about menopausal women is that they cannot build muscle after a certain age. The argument goes that as certain hormones decline, so too does the ability to build muscle. On the surface, that seems like a reasonable argument. Indeed, there have been an endless number of studies that suggest hormone decline, in both males and females, negatively influences muscle mass and strength. Ditto for the opposite – increasing certain hormones increases muscle development for both males and females. Why else would we have entire industries devoted to the development of hormones for use in competitive sports and sub-industries whose sole purpose is to find ways to circumvent the detection of those products? Yes, all else being equal, certain hormones impact muscle development more positively in higher concentrations and more negatively in lower concentrations. Does that mean however that hormones are the sole contributors to muscle development, or as the menopausal research always seems to conclude, that the state of diminishing hormone concentrations as we age and move through menopause is enough to hamper or prevent muscle development in women? No. Absolutely not.
Like so many aspects of women’s health research, the connection between declining hormones and declining muscle is spurious at best. It relies on equal parts latent (and no so latent) biases towards women and surrogate markers that may or may not equate directly with muscle and strength. The bias holds that women in general have difficulty building muscle compared to men based upon their unique hormonal makeup e.g. lower androgens and higher estrogens, a difference that is magnified with aging. This bias leads to research questions that essentially presume the answer in the framing of the question. That is, the research asks ‘why women have difficulty building muscle’ across menopause or compared to men and not ‘do women have difficulty building muscle.’ The research assumes that women have this issue, and thus, proceeds show us why. It then uses surrogate markers of this supposed muscle building difficulty, neither defining clearly what constitutes muscle development nor measuring actual muscle development in women who train to build muscle. When the associations between these surrogate markers and the hormone in question is found, usually estradiol, are found, as they so often are, causation is inferred and PR campaigns begin.
This bugs me to no end for a number of reasons, not the least of which, because it is an asinine way to conduct research, but mostly, because it is logically fallacious. We have made the assumption that women have difficulty building muscle and proceed to demonstrate why. Of course, we are going to find some reasons. We can do that with any research design that assumes the answer in the question. It would be no different than assuming all men idiots and designing research to find out why. It is offensive and it is wrong, and yet, this is the standard course of most research. What is that saying – assumptions make asses out of you and me? Well, research like this makes asses out of us all.